Yingjia Huang, DHCS Deputy Director for Health Care Benefits and Eligibility
Statewide — California health leaders are preparing for sweeping changes to Medi-Cal, the state’s version of Medicaid, that will affect millions of residents over the next three years.
During a Sept. 11 virtual media briefing hosted by American Community Media, officials from the California Department of Health Care Services (DHCS) detailed upcoming federal and state policy shifts that will impact eligibility, benefits andcosts for the more than 15 million Californians who rely on Medi-Cal.
“These policies can carry real consequences for the lives of Medi-Cal members,” said Tyler Sadwith, California’s stateMedicaid Director. “We are committed to sharing information so that Californians can make informed decisions for themselves and their families.”
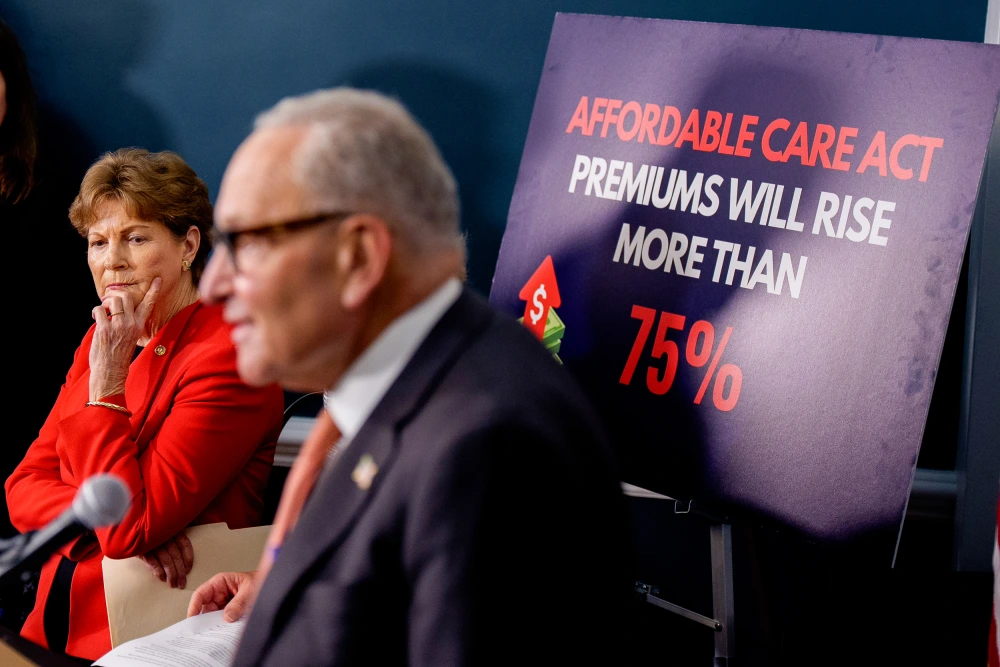
Sadwith explained that a recently passed federal law, sometimes referred to as the “One Big Beautiful Bill,” introducesstrict new rules for Medicaid programs nationwide starting in Jan. 1, 2027.
One major provision requires some adults between ages 19 and 64 to work, attend school, participate in job training or volunteer at least 80 hours a month to keep their coverage.
Exemptions include children, seniors aged 65 and older, pregnant individuals for one year postpartum, people withdisabilities, caregivers of children under 14, and several other groups.
“If a Medi-Cal member is required to work or volunteer under these new federal rules and they do not meet the rules, they could lose their Medi-Cal coverage,” Sadwith said.
The law also requires certain members without dependent children to renew eligibility twice a year instead of annually, starting in January 2027.
Additionally, beginning in October 2028, some adults may face small copayments for specialty care and tests, though core services like emergency care and mental health treatment will remain free.
“These new work requirements will be hard for some adults to meet, especially those with unstable or seasonal jobs,” Sadwith warned.
He added that the state estimates up to 3.4 million Medi-Cal members could be at risk of losing coverage due to the combined effects of the new federal requirements.
Yingjia Huang, DHCS Deputy Director for Health Care Benefits and Eligibility, outlined several state budget-driven changes beginning in 2026.