While some people with a COVID-19 infection may experience relatively mild symptoms (or no symptoms at all), the disease is of greater concern for the 56% of Americans who may have at least one risk factor linked to an increased chance of complications.
Two increasingly common risk factors for COVID-19 are obesity and type 2 diabetes, which in some cases may be improved or even reversed with appropriate lifestyle modifications. As the COVID-19 situation evolves, it is important to recognize that daily decisions related to diet and activity may make a difference in the severity of infection. Research shows people with existing diabetes whose blood sugar is well controlled may require fewer medical interventions and are more likely to recover from COVID-19.
With health now top of mind for many Americans, hopefully these challenging times can serve as a spark to help our nation address its long-standing chronic disease epidemic, which affects more than 196 million people and accounts for over $3 trillion in annual health care costs.
Here are tips to consider related to obesity and type 2 diabetes amid the COVID-19 pandemic:
Monitor your body mass. While body mass index (BMI) has potential shortcomings, especially for athletes such as weightlifters, this calculation of height compared to weight may provide a helpful measure to monitor. In fact, people with even moderately elevated BMI levels may have an increased risk of developing complications related to diabetes. To monitor your BMI, check with your primary care physician or use an online calculator.
Use interval eating. The cliché “you are what you eat” may ring true when it comes to preventing or managing obesity and diabetes, but when and how you eat also may be relevant. Also called intermittent fasting or time-restricted eating, this approach alternates periods of fasting and non-fasting during the day or across the week. Lifestyle changes to consider include waiting at least an hour after waking up before eating breakfast and avoiding food within three hours of sleep. In addition, people may consider the order in which they eat food, starting each meal with a lean protein (chicken, fish or turkey), followed by a vegetable (asparagus, broccoli or carrots) and ending with a carbohydrate (beans, brown rice or sweet potato). This ordered approach may lead to lower post-meal glucose and insulin levels for people with type 2 diabetes. People interested in this approach to eating should discuss it with their health care provider, as medication regimens may need to be adjusted.
After-meal walks. People seeking to better control their blood sugar levels and weight should also consider short walks after eating meals or snacks, especially those with added sugars that may be contained in juice or desserts. Post-meal walks may help the body move sugar from the blood into muscle cells, helping normalize blood sugar levels. Whenever possible, make time for a 15-minute walk after each meal to help reduce the risk of blood sugar spikes.
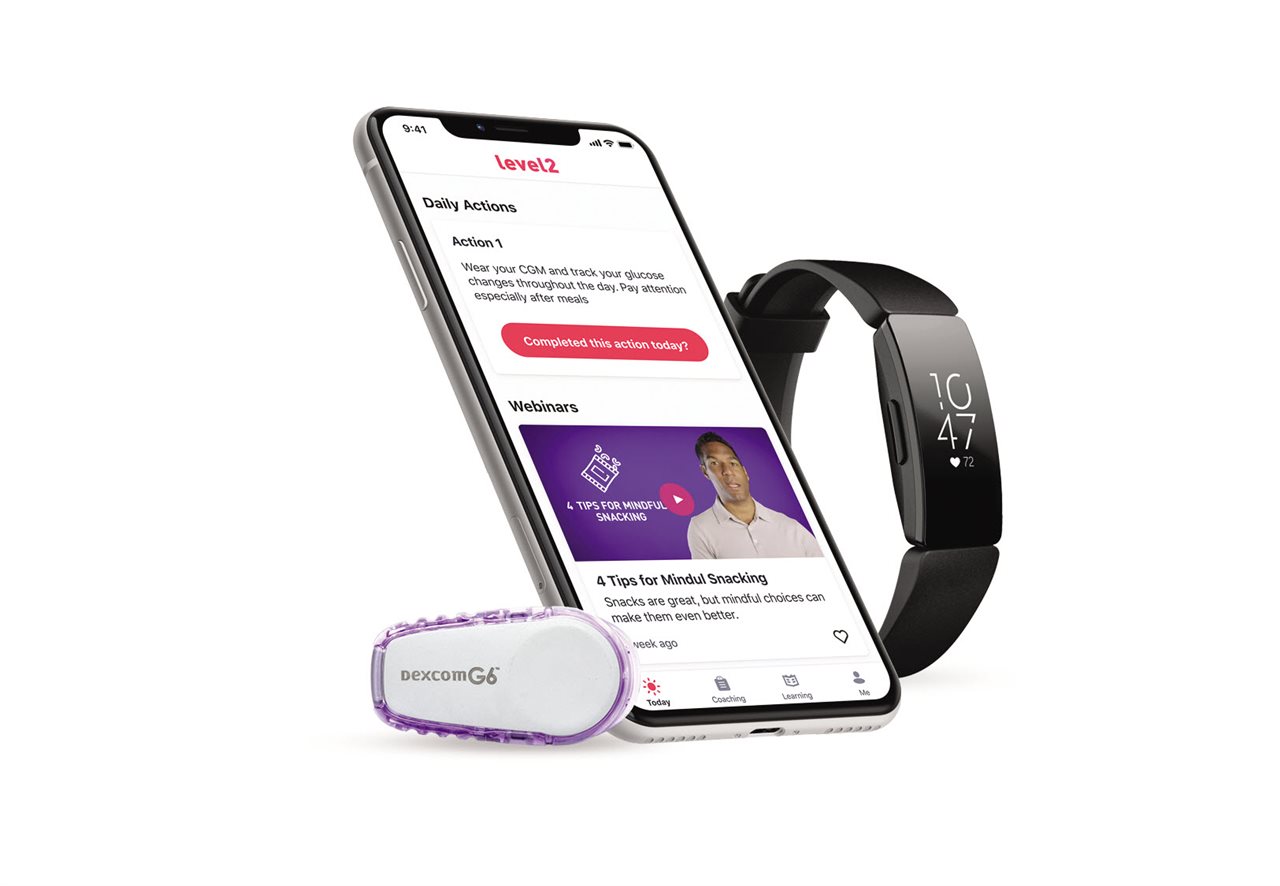
Take advantage of technology. Smartwatches and activity trackers are potential resources to help monitor various health measures, including daily steps, sleep patterns and blood sugar levels. Recently, some people with diabetes have started using continuous glucose monitors. This technology, which uses a sensor often worn on the abdomen, continuously reads glucose levels and transmits the data to a smartphone. This may give users and health care providers important information in real time, helping reveal relationships between eating, exercise and blood sugar that may be difficult to observe with only test strips and a glucose meter. While these devices may cost $500 or more and require a prescription, health plans such as UnitedHealthcare are starting to provide these at no additional cost to members as part of diabetes management programs.
“Connected devices such as continuous glucose monitors and activity trackers may be game changers for the approximately 30 million people nationwide living with type 2 diabetes,” said Dr. Donna O’Shea, chief medical officer of population health management, UnitedHealthcare. “By considering these tips, these challenging times may serve as a catalyst for people to help improve their health and reduce the possible risk of complications from COVID-19.”
Information provided is for general purposes only and is not intended to be construed as medical advice; people should consult an appropriate health care professional to determine what may be right for them. –BPT