Dr. Lenore A. Tate
Licensed clinical psychologist Dr. Lenore A. Tate has spent decades helping individuals and communities understand the long-term effects of trauma and the pathways toward healing.
Based in Sacramento, Tate earned her Ph.D. from the California School of Professional Psychology–Fresno, a master’s degree in psychology from Howard University, and a bachelor’s degree in psychology from Mills College.
Her work centers on culturally competent, trauma-informed care, with a growing focus on how unresolved trauma shows up in the body and mind as people age.
As she puts it, “Belongingness is the E-ticket to mental well-being.”
Dr. Tate spoke with California Black Media (CBM) recently. During that conversation, she unpacked the complex relationship between trauma, health, belonging, and resilience.
What is trauma?
Trauma can be a deeply disturbing or distressing experience that can have a significant impact on an individual, a family and/or community. I like to look at trauma from three prongs:
First, psychological trauma which results from abuse, violence, accidents, natural disasters, loss, or prolonged stress; Second, physical trauma, which can be a bodily injury; and, finally, collective or cultural trauma, which is caused by a major event like war, displacement, and systemic oppression and which affects an entire group.
Today, the mental health field recognizes the importance of a cultural lens, because collective trauma has a ripple effect on the individual, family and community.
Why do people say that trauma is “in the body?”
Regardless of your age, trauma shows up in the body. It could be cardiovascular strain, high blood pressure, digestive issues, ulcers, chronic constipation and more. People might not know that even constipation or diabetes may be connected to a trauma. It can also lead to cognitive decline, a weaker immune system and accelerated aging.
How can people cope with trauma?
There are many ways to be resilient and regulate our feelings from therapy to self-help/care to connections with others to developing coping mechanisms and caring for your physical health. Some people exercise, read poetry, journal, or draw. When I was stressed out as a kid, my mom taught me how to breathe and take deep breaths in and breathe out. I also learned to keep track of my own body cues.
People can also seek to understand and address the trauma through mental health care,which is just as important as physical health care. Employer-based health insurance usually includes mental health. Many workplaces offer an employee assistance program (EAP) that offers free counseling. There are hotlines and warmlines for parents, seniors and many other groups. You can call 211 and tell them what kind of support you are looking for. There are also a growing number of free self-help groups for the Black community called healing circles, and today, many barbers and hairdressers have also received some training.
What does emotional regulation feel like?
For me, it’s a state of being, and the ability to manage feelings between the highs and the lows of our emotions. It’s a sense of internal safety, homeostasis, the baseline. It’s the ability to be aware of our emotions, understand our feelings and thoughts (and manage them) and find healthy ways to express our emotions.
How do we get to mental health and wellness?
Belongingness is the E-ticket to mental well-being. If you have a sense of connectedness, a sense of collective unity, friends, a church, a bid whist group, then you have some of the strongest resilience factors from mental disorders and substance use.
As we age, do we have to search for new spaces of belonging?
As people age, they can lose their routine, their purpose, and their people. They’re no longer raising children or working, and their universe has become narrower, so they have to make a conscious effort to be intentional. My tip is to choose three activities that you love, whether they’re online or in person, and go consistently for at least six sessions. After six sessions, you begin to develop a sense of community
What is the connection between substance use and trauma?
Trauma is a major risk factor for substance use. One primary contributing factor is that trauma dysregulates the brain, which makes substance use behaviors more frequent.
There are some ethnic groups, particularly African Americans, whose pain has been minimized by the medical community, so their pain has not been adequately treated. At the same time, there has been overuse of pain and other medications to lessen anxiety or depression. The nexus between trauma and substance use is real and dangerous for everyone and especially seniors. Over the last 20 years, the rate of fentanyl mortalities among seniors has increased 400%.
People often know what will make us healthier, but we don’t do it. Why is that?
We don’t really love on ourselves the way we would a partner or family member. We’re putting work, our kids, our caregiving, before ourselves. On the airplane, they say, put your oxygen mask on yourself first. We need to commit to our well-being first and we also need to explore, mentally, how to move forward.
What is in your mental health toolkit?
1) Belonging and strong social connections
2) Having or searching for purpose or meaning in your life
3) Emotional awareness of your feelings and thoughts.
4) Access to culturally competent trauma-informed mental health care
5) Having multiple plans and strategies. For example, when you go into a difficult situation, have a Plan A and if that doesn’t work, go to Plan B.
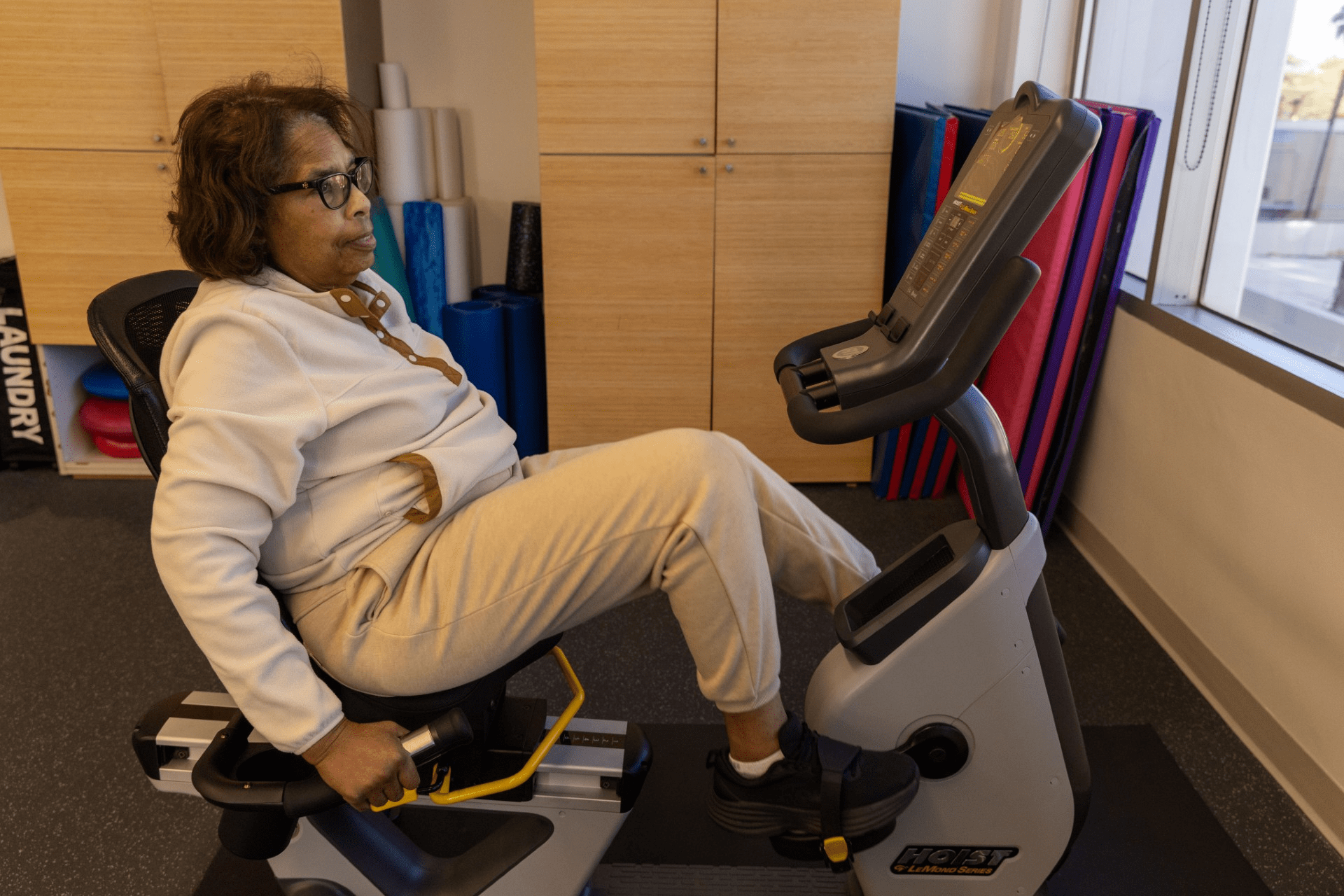
6) Exercise, which could be a walk.
7) A good, healthy diet.
8) An understanding of my health profile: blood pressure, cholesterol and even my ACE (adverse childhood experience) score, which is the number of traumatic events I had as a child.
9) At least 2 friends who will check on me if they haven’t heard from me in three days.
10) Something sensory, like music, aromas, a favorite blanket.
11) The proverbial oxygen mask and the commitment to put the mask on myself first.
______________
Article By: Amanda Kim, California Black Media